Glaucoma
What is Glaucoma?
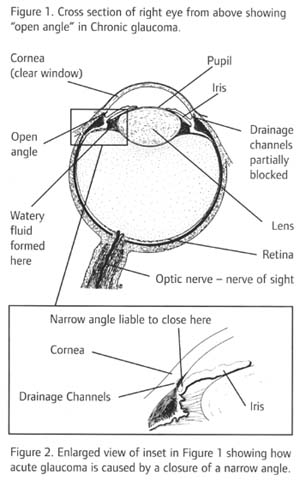
Glaucoma is the name for a group of eye conditions in which the optic nerve is damaged at the point where it leaves the eye. As the diagram shows, this nerve carries information from the light sensitive layer in your eye, the retina, to the brain where it is perceived as a picture.
Your eye needs a certain amount of pressure to keep the eyeball in shape so that it can work properly. In some people, the damage is caused by raised eye pressure. Others may have an eye pressure within normal limits but damage occurs because there is a weakness in the optic nerve. In most cases both factors are involved but to a varying extent.
Eye pressure is largely independent of blood pressure.

What controls pressure in the eye?
A layer of cells behind the iris (the coloured part of the eye) produces a watery fluid, called aqueous. The fluid passes through a hole in the centre of the iris (called the pupil) to leave the eye through tiny drainage channels. These are in the angle between the front of the eye (the cornea) and the iris and return the fluid to the blood stream. Normally the fluid produced is balanced by the fluid draining out, but if it cannot escape, or too much is produced, then your eye pressure will rise. (The aqueous fluid has nothing to do with tears.
Why can increased eye pressure be serious?
If the optic nerve comes under too much pressure then it can be injured. How much damage there is will depend on how much pressure there is and how long it has lasted, and whether there is a poor blood supply or other weakness of the optic nerve. A really high pressure will damage the optic nerve immediately. A lower level of pressure can cause damage more slowly, and then you would gradually lose your sight if it is not treated.
Are there different types of glaucoma?
Yes. There are four main types.
Chronic glaucoma
The most common is chromic glaucoma (chronic = slow) in which the aqueous fluid can get to the drainage channels (open angle) but they slowly become blocked over many years (see figure 1). The eye pressure rises slowly and there is no pain to show there is a problem, but the field of vision gradually becomes impaired.
Acute glaucoma
Acute glaucoma (acute = sudden) is much less common in western countries. This happens when there is a sudden and more complete blockage to the flow of aqueous fluid to the eye. This is because a narrow 'angle' closes to prevent fluid ever getting to the drainage channels (see figure 2). This can be quite painful and will cause permanent damage to your sight if not treated properly.
Secondary and developmental glaucoma
There are two other main types of glaucoma. When a rise in eye pressure is caused by another eye condition this is called secondary glaucoma. There is also a rare but potentially serious condition in babies called developmental or congenital glaucoma which is caused by malformation in the eye. This article is about chronic and acute glaucoma.
How common is glaucoma?
In the UK some form of glaucoma affects about 2 in 100 people over the age of 40.
Are some people particularly at risk of chronic glaucoma?
Yes. There are several factors that increase the risk.
Age
Chronic glaucoma becomes much more common with increasing age. It is uncommon below the age of 40 but affects one per cent of people over this age and five per cent over 65.
Race
If you are of African origin you are more at risk of chronic glaucoma and it may come on somewhat earlier and be more severe. So make sure that you have regular tests.
Family
If you have a close relative who has chronic glaucoma then you should have eye tests at intervals. You should advise other members of your family to do the same. This is especially important is you are aged over 40 when tests should be done every two years.
Short sight
People with a high degree of short sight are more prone to chronic glaucoma.
Diabetes
Diabetes is believed to increase the risk of developing this condition.
Please note: People over the age of 40 years and with a family history of glaucoma - such as parents, children or siblings of people diagnosed with glaucoma - are entitled to a free sight test every 2 years under the NHS.
Why can chronic glaucoma be a serious risk to sight?
The danger with chronic glaucoma is that your eye may seem perfectly normal. There is no pain and your eyesight will seem to be unchanged, but your vision is being damaged. Some people do seek advise because they notice that their sight is less good in one eye that the other.
The early loss in the field of vision is usually in the shape of an arc a little above and/or below the centre when looking 'straight ahead'. This blank area, if the glaucoma is untreated, spreads both outwards and inwards. The centre of the field is last affected so that eventually it becomes like looking through a long tube, so-called 'tunnel vision'. In time even this sight would be lost.
How is chronic glaucoma detected?
As glaucoma becomes much more common over the age of forty you should have eye tests at least every two years and ask for all three glaucoma tests. This has been shown to be much more effective in detecting glaucoma than just having one or two of the tests.
These tests are:
- Viewing your optic nerve by shining a light from a special electric torch into your eye.
- Measuring the pressure in the eye using a special instrument.
- Being shown a sequence of spots of light on a screen and asked to say which ones you can see.
All these tests are very straightforward, don't hurt and can be done by most high street optometrists (opticians).
How is chronic glaucoma treated?
The main treatment for chronic glaucoma aims to reduce the pressure in your eye. Some treatments also aim to improve the blood supply to the optic nerve. You will need to go to hospital for treatment and have regular check-ups afterwards.
Treatment to lower the pressure is usually started with eyedrops. These act by reducing the amount of fluid produced in the eye or by opening up the drainage channels so that excess liquid can drain away. If this does not help, your specialist may suggest either laser treatment or an operation called a trabeculectomy to improve the drainage of fluids from the eye.
Your specialist will discuss with you which is the best method in your particular case.
Can chronic glaucoma be cured?
Although damage already done cannot be repaired, with early diagnosis and careful regular observation and treatment, damage can usually be kept to a minimum, and good vision can be enjoyed indefinitely.
What is acute glaucoma?
In acute glaucoma the pressure in the eye rises rapidly. This is because the periphery of the iris and the front of the eye (cornea) come into contact so that aqueous fluid is not able to reach the tiny drainage channels in the angle between them. This is sometimes called closed angle glaucoma (see figure 2).
What are the symptoms of acute glaucoma?
The sudden increase in eye pressure can be very painful. The affected eye becomes red, the sight deteriorates and may even black out. There may also be nausea and vomiting. In the early stages you may see misty rainbow coloured rings around white lights.
Is acute glaucoma always severe?
Sometimes people have a series of mild attacks, often in the evening. Vision may seem 'misty' with coloured rings seen around white lights and there may be some discomfort in the eye. If you think that you are having mild attacks you should contact your doctor without delay. In routine examinations the structure of the eye may make the examiner suspect a risk of acute glaucoma and advise further tests.
What is the treatment?
If you have an acute attack you will need to go into hospital immediately so that the pain and the pressure in the eye can be relieved. Drugs will be given which both reduce the production of aqueous liquid in the eye and improve its drainage.
An acute attack, if treated early, can usually be brought under control in a few hours. Your eye will become more comfortable and sight starts to return. When the pain and inflammation have gone down, your surgeon will advise making a small hole in the outer border of the iris to relieve the obstruction, allowing the fluid to drain away. This is usually done by laser treatment or by a small operation.
Usually the surgeon will also advise you to have the same treatment on the other eye, because there is a high risk that it will develop the same problem.
This treatment is not painful. Depending on circumstances and the response to treatment, it may not require admission to hospital. Sometimes a short stay in hospital may be advised.
Can acute glaucoma be cured?
If diagnosed without delay and treated promptly and effectively there may be almost complete and permanent recovery of vision. Delay may cause loss of sight in the affected eye. Occasionally the eye pressure may remain a little raised and treatment is required as for chronic glaucoma.
Will I be able to drive?
Most people can still drive if the loss of visual field is not advanced. To assess possible damage to your peripheral vision you will need a special test to see whether your sight meets the standards of the Driver and Vehicle Licensing Authority. Ask you specialist about this.
What if my sight cannot be fully restored?
Early detection and treatment will usually prevent or retard further damage by glaucoma. Much can be done to help you use your remaining vision as fully as possible. You should ask your optician of optometrist about low vision aids and whether you are eligible to register as partially sighted or blind. Registration opens the door to expert help and sometimes to financial benefits.
All information is for reference purposes only; if you have any concerns we recommend that you visit a qualified optician.
Related Eye Condition Links:
Blepharitis;
Cataracts;
Colour-Blindness;
Conjunctivitis;
Corneal Abrasion;
Dry Eyes;
Ectropion;
Entropion;
Iritis / Uveitus;
Keratoconus;
Laser Treatment;
Macula Degeneration;
Meibomian Cyst;
PVD;
Short Sightedness.
Return to Information & Eye Tests.
Please note that the content on this website is for information purposes only and is not a substitute for professional medical advice. Please consult your doctor or optician particularly if you are already under medical care.